Plumbing designs make health care facilities safer places to convalesce
Patient safety on tap

Adding tools to a health care facility’s plumbing arsenal will help address challenges for patients, staff and health care facility management. Photos courtesy of Chicago Faucet.
Medical facility managers face the challenges of managing the building and keeping patients or residents safe from health care acquired waterborne infections, self-inflicted injury and scalding.
Everyone hopes when going to the hospital or nursing home they come out well. Sadly, that is not always how things work out.
This mission is of significant concern for owners and operators. The U.S. Centers for Disease Control and Prevention (CDC) estimates that 5% of all hospital admissions result in a health care-associated infection, culminating in approximately 722,000 infections and 75,000 deaths annually, and $28-$33 billion in excess costs.
Engineers who specify plumbing fixtures for hospitals and senior housing projects must select the most effective products to manage risk. To address water risks, the American National Standards Institute (ANSI)/American Society of Heating, Refrigerating, and Air Conditioning Engineers (ASHRAE) introduced a new standard in July 2023. ASHRAE 514, Risk Management for Building Water Systems: Physical, Chemical, and Microbial Hazards, provides a framework to handle disease outbreaks and hazards that could become public health and safety issues.
ASHRAE 514 creates an industry standard to prevent both illness and injury. It is important that facility managers becoming familiar with the ASHRAE 514 standard and how to implement it to manage risk. The Centers for Medicare & Medicaid Services (CMS) requires Water Management Program for every type of health care facility, while individual states have taken it in their hands to include additional housing facilities.


Smarter faucets mean safer patients and health care staff. If a user doesn’t touch a faucet, the opportunity for cross-contamination is significantly reduced, if not eliminated. Photo courtesy of Chicago Faucet
Stagnant water — sending infections down the drain
The problem
In a health care or nursing home setting, water is everywhere because it plays a significant therapeutic and hygienic role. But lurking in the pipes is the danger that they can carry infectious pathogens should the water become stagnant thus compromising patient or resident immune systems. Health care facilities are subject to a host of infections but in particular with water stagnation is Legionella.
Of key concern is the stagnant water in the shower system of patient rooms. The shower hose and the water in the pipes may only partially drain after repeated use. Having nurses’ aides drape shower hoses into the shower stall to drip out water does not fully drain the water and creates additional safety hazards not to mention the extra time.
The solution
Nurses as well as facility managers have been seeking alternate ways to remove the manual drop of the hose. There are now methods for anti-stagnation to retrofit existing showers or build it in with new shower construction. For retrofit, specialty shower hoses can automatically drain standing water in the shower hose with a special drain assembly. After each use, water drains automatically from the hand spray and hose via drain assembly that is integrated into the hose that allows the water to easily flow out. This design eliminates draping the hose where it could touch the floor and risk further contamination.
For new construction, the water column behind the wall can also be drained with an automatically draining valve that removes stagnant water in the shower column. Water drains automatically from the shower system at shut-off in under a minute. This function can be available as a separate remote drain or integrated into the shower trim.
For multi-spray showers, a diverter is also available so both the shower head and column as well as the hose and hand spray are properly drained. With low to no use comes the realization that the pipes are not being flushed regularly causing concern for infection.
Limiting infections with touch-free faucets specifically for health
The problem
Staff use water for patient treatment and best practices suggest washing their hands with soap and water before and after each patient encounter, especially if they are touching surfaces. One surface that demands attention is the handles on faucets. Influenza, salmonella, e-coli, C. diff and many other germs could be in the midst.
The problem with washing your hands of these sources for illness is using faucets with handles. A Special Pathogens Lab study found that on faucet handles in one healthcare facility, a faucet handle can be the home of over 2,000 bacteria colony-forming units. Faucet handles can transmit from person-to-person germs such as influenza, salmonella, and the common cold.
In the surgical and intensive care rooms, handwashing is paramount and having the right electronic faucet makes a difference. Not all automatic faucets are created equal.
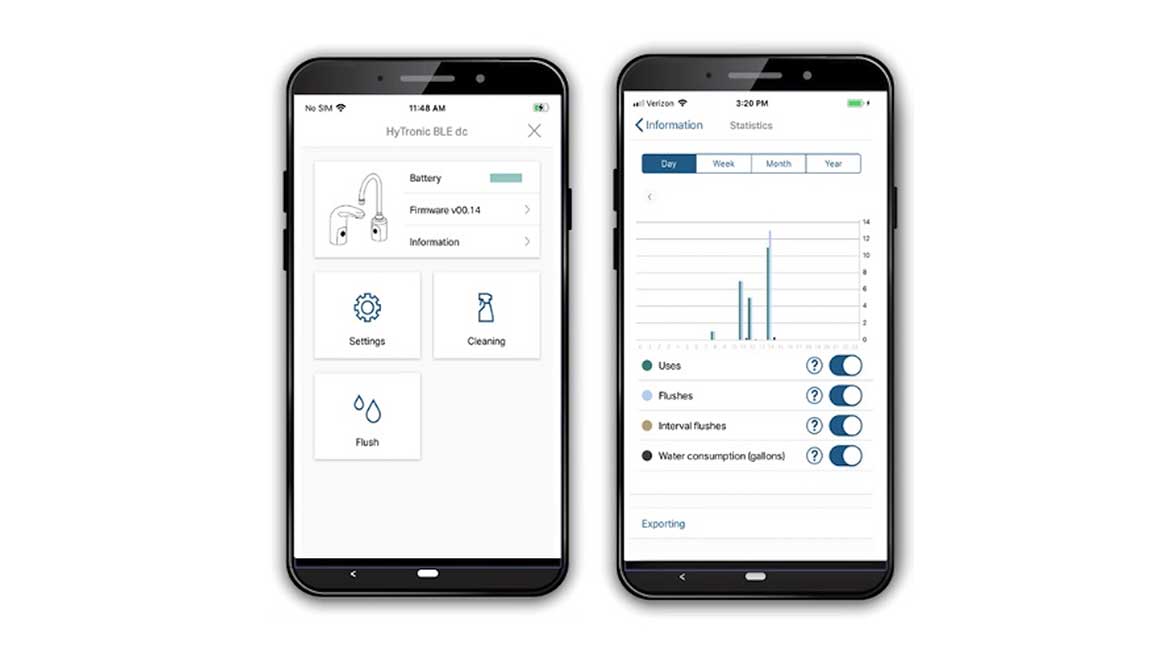
Apps allow facility maintenance staff to determine operational status, water temperature, faucet and pipe flushing and water usage to save water and additional resources. Photo courtesy of Chicago Faucet
The solution
Hygienic sensor faucets mean safer patients and medical staff.
If a user doesn’t touch a faucet, the opportunity for cross-contamination is significantly reduced if not eliminated. Touchless electronic faucets enable both the medical staff and the patients to avoid contact with the handle and are an alternative to a traditional, manually operated faucet. It can sense motion and turn on the water automatically, keeping bacteria off hands. For medical personnel, these faucets can meet Centers for Disease Control handwashing guidelines.
For a touchless faucet to earn its place, the sensor in the faucet must deliver water at the right temperature quickly and stop flowing when the user withdraws hands to save water. Faucets designed for health care go beyond simply dispensing water and they make it easier for facilities management.
- To minimize infections, look at specifying dual cross beam sensor faucets that offer antimicrobial laminar outlets, copper inlet tubes, commercial grade check stops to prevent cross flow and an ASSE1070 certified thermostatic temperature control that allows waterways and valves to be flushed without the need for a separate bypass line to the faucet when flushing. And be assured that they keep running with a long term or emergency battery power.
- Water management made easy. Facilities managers can reduce water stagnation and remove harmful bacteria in these faucets with a mobile phone app that offers Hygiene that Flush modes: use-based, interval-based and volume-based options.
Ouch, that was hot!
The problem
In nursing and other multi-family centers, the facilities team may turn up the water to kill the bacteria in the line, however, the thermostatic mixer for the faucet or shower may be far away from the point of use. Staff and aides need to be observant so their residents don’t scald themselves while hand washing or showering.
ASHRAE 514 addresses physical hazards like water scalding. Children and seniors with thinner skin are more prone to it and this results in deeper burns for the same temperature and exposure time. To alleviate risk, the U.S. Consumer Product Safety Commission recommends lowering the water heater temperature to 120° F.


Ligature prevention faucets must not have any ligature points, so manufacturers have come out with rounded and sloped designs that meet those needs, yet are touchless and easy to operate. This design resists the attachment of bed sheets, cords or any other material that may result in injury or loss of life yet makes running water easy to access. Photo courtesy of Chicago Faucet
The solution
Although turning down the water temperature to 120° F to avoid scalding saves the energy needed to heat water, microbes like Legionella can survive several hours at this temperature. Installing thermostatic mixing valves as close as possible to point of use helps to prevent scalding. Storing hot water at temperatures above 140° F and circulate continuously above 120° F, is recommended per the CDC. Use pipe insulation to maintain hot and cold water at desired temperatures throughout the water system.
ASSE 1070 Certified Valves for Faucets — valves must be thermostatic and provide scald protection at the rated flow rate of the fixture. Faucets can have an integrated thermostatic design or water can be tempered using an add-on valve. The valve must be set to deliver a maximum water temperature of 120° F or less. For non-adjustable water temperature fixtures the outlet temperature must be 110 F or less.
ASSE 1016 For Tubs/Showers — Valves can be pressure-balancing, thermostatic or combination pressure-balancing/thermostatic. In-line thermostatic valves may not be utilized to meet this standard. Valves must provide scald and thermal shock protection for the rated flow rate of the installed shower head. The valve must limit the maximum setting to 120° F and have a maximum temperature limit stop set prior to occupancy. The limit stop must be checked and adjusted seasonally to reflect changes in cold water temperature.
A healthy dose of safety for health care
With industry and government agencies mandating infection control measures and patient safety environments, plumbing manufacturers are focused on creating products that help facilities do their jobs of achieving positive outcomes for their patients.
Knowing which plumbing fittings are ideal for each type of project requires working with a knowledgeable plumbing products manufacturer’s representative. Engineers that meet specifications can exceed customer expectations by delivering health care facilities that truly provide a positive healing experience for patients, caregivers, long-term care residents and staff.
Looking for a reprint of this article?
From high-res PDFs to custom plaques, order your copy today!