LEED In Healthcare
Healthcare buildings (hospitals, nursing homes and outpatient centers) are unique buildings. They hold a special place in our culture and communities. They are centers for healing and wellness, and places where people and their families gather to receive comfort, celebrate and mourn.

Because healthcare buildings have such significant effects on the environment (indoor, community and global) (see Figure 1), the U. S. Green Building Council has recognized the value of providing a tool that is tailored to apply the LEED system to healthcare construction. The LEED Application Guide for Healthcare is currently under development, and is generally based on the Green Guide for Health Care (for more information, visit www.gghc.org).
That is not to say that the current version of LEED-NC is inapplicable to healthcare design and construction. The USGBC estimates that about 50 healthcare buildings are currently pursuing LEED certification, under the current LEED-NC product, and at least one of those is seeking Platinum- level certification. At the time of the writing of this article, two healthcare buildings (Foothills Community Hospital Boulder, Colo., and the Patrick H. Dollard Discovery Health Center in upstate New York) have achieved LEED certification. The Application Guide for Healthcare is meant to provide more credits that are specifically suited for healthcare projects, with particular attention to the improvement of health outcomes associated with those measures.
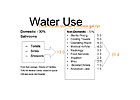
In the Water Efficiency category, The Application Guide pays special attention to the reduction or elimination of the so-called “process” uses of potable water, since it is estimated that more than two-thirds of the potable water used in a hospital is used for these processes (see Figure 2). Some strategies and measures that can be employed to achieve the desired reduction include:
LEED emphasizes adherence to ASHRAE Standard 90.1-2004-Energy Standard for Buildings Except Low-Rise Residential Buildings. In most jurisdictions, state licensing boards have not required adherence to an energy code (though some jurisdictions require the building envelope meet some level of insulation performance), so the specialized healthcare designer may not know its requirements. One of the most significant power limitations for mechanical systems is the fan power limit. Standard 90.1 limits the total system fan power (includes supply, return, and exhaust fans). For constant volume systems smaller than 20,000 cfm in supply volume, total system fan power is limited to no more than 1.2 hp/1,000 cfm. For constant volume systems equal to or greater than 20,000 cfm, the limit is reduced to 1.1 hp/1,000 cfm. For variable volume systems, the limits are increased to 1.7 hp/1,000 cfm and 1.5 hp/1,000 cfm for the small and large systems, respectively. Systems that use high-efficiency final filtration are allowed a power adjustment based on pressure drop through clean filters. These fan power limitations will mean careful and efficient duct system design to reduce pressure drops.

While it may seem that LEED is harder to achieve in a healthcare building, some LEED credits are relatively easy to achieve for buildings that already must comply with a rigorous licensing standard. For instance:
One Indoor Environmental Quality credit that may trip up mechanical and plumbing specifiers is the requirement for low-emitting sealants and adhesives. To achieve this credit, any adhesives or sealants that are used inside the conditioned envelope of the building must comply with California's South Coast Air Quality Management District Rule No. 1168. While this requirement has been in force in California since before the turn of the millennium, this may come as a surprise to many non-West Coast mechanical and plumbing installers, particularly those using mastics and adhesives in caulking, firestopping, duct construction and insulation.
The draft mission statement of the Application Guide for Healthcare carries an important message for plumbing and mechanical designers and installers - “By affirming healthcare's fundamental mission of ' … first, do no harm,' the Application Guide for Healthcare recognizes the profound impact of the built environment on the health of occupants, local communities and global ecology, and encourages design strategies that enhance the healing environment for patients, healthy and productive work environments for staff, and responsible ecological stewardship.”
Looking for a reprint of this article?
From high-res PDFs to custom plaques, order your copy today!








