
Based on projections by the U.S. Census Bureau, the number of Americans beyond the age of 65 will more than double from the year 2000 until 2030.
What that means for the building industry is that as America gets older, the demand for healthcare will increase. You can further conclude that contractors with expertise in this already hot market will be in demand for years to come.
Take a look at the American Institute of Architects' proposal, “Guidelines for Designs and Construction of Hospital and Healthcare Facilities,” which can be downloaded online at www.aia.org/aah_gd_hospcons.
According to the proposals, a demand for healthcare hygiene requires each retrofit patient room be provided a hand-washing station to service it and each new-construction patient room will include its own hand-washing station (17.2.A45).
Hand-washing stations are also required at nursing stations, in examination rooms and in “clean” storage areas that contain items to be prepared for patient care (27.2.B11).
The AIA's spec-driven guidelines further state that each patient shall have access to a toilet room without having to enter the general corridor area. Furthermore, the toilet room shall serve no more than four beds and no more than two patient rooms. These toilet rooms must contain a water closet, as well as a hand-washing station (37.2.A56).
The broad AIA specifications proposed for just this portion of healthcare space show that there will be significant opportunity for plumbing contractors. But added to that are public restroom facilities, not to mention other water-consuming fixtures needed to operate a healthcare facility.
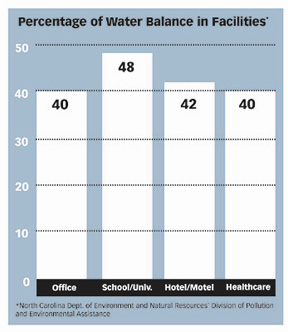
Because 40 percent of the water used in hospitals is consumed by washing, bathing and flushing, restrooms are the most obvious area where water conservation objectives can be reached. In fact, potable water consumption reductions may be achieved through the use of “low consumption fixtures and controls,” according to the Water Conservation section (4A2.3C).
In this important section, the AIA refers to the growing body of knowledge for sustainable construction - namely the U.S. Green Building Council's LEED Green Building Rating System and Green Guidelines for Healthcare Construction - available to assist building professionals and healthcare organizations in understanding how structures affect human health and the environment, and how these effects can be mitigated through a variety of strategies.
Water Conservation: A program like LEED establishes “best practice” criteria for water and energy usage, materials and indoor environmental quality. It is not exclusive to universities, city halls or R&D centers of large corporations, but healthcare facilities, too. As proven with the two LEED healthcare projects5 - and many others registered for consideration - plumbing contractors who can maximize point earnings will be in demand.
LEED provides a checklist of green building measures in specific categories:
- Sustainable Sites, which includes credits for controlling soil erosion as well as considerations to reduce overall site disturbance.
- Energy and Atmosphere, which includes credits for optimizing energy performance and incorporates credits for use of renewable technologies.
- Materials and Resources, which offers credits for a range of sustainable design strategies, including the use of recycled building materials.
- Indoor Environmental Quality, which includes ways to establish minimum indoor air quality performance and occupant comfort and health.
- Water Efficiency, which includes ways to maximize water efficiency both in outside irrigation as well as indoor water usage.
- Innovation and Design Process, which addresses design measures not covered in the other categories.
One of the simplest ways to earn LEED credits is by surpassing the standards for water efficiency. That means reducing water consumption 20 percent below the baseline fixture performance requirements set by the Energy Policy Act of 1992 for one point or reducing consumption by 30 percent in comparison with the baseline for two points.
By far, the most affordable area to focus on is the restroom. According to the U.S. Department of Energy, the Water Efficiency LEED category can contribute tremendously to the bottom line, making the specification of efficient fixtures very cost-effective over the life cycle of the facility.
For example, a baseline toilet fixture uses 1.6 gallons per flush and a baseline urinal consumes 1 gpf. Consider then the fiscal and environmental impact of a strategy that uses 0.5 gpf urinals or even waterless urinals and ultra low-flush toilet fixtures that use 1 gpf.
But the largest source of restroom water savings comes from sensor-operated lavatory faucets with 0.5 gallon-per-minute aerators. These green products reduce consumption because water flows only when a person's hands are in the “active area,” meaning that while the user lathers or dries their hands, water flow stops, minimizing waste.
Citing hand-washing as the single most effective method to reduce illness and cross-contamination, the Centers for Disease Control and Prevention's recommended healthcare hand-washing protocol states that a person should wet hands first with water, apply the amount of soap recommended by the manufacturer, and rub hands together for at least 15 seconds, covering all surfaces of the hands and fingers. A person should then rinse their hands with water, dry thoroughly with a disposable towel, and use the towel to turn off the faucet.
Notably, the last instruction was to turn off the faucet, which indicates that water was flowing down the drain and being wasted during the entire hand-washing process. With an estimated 56 minutes spent washing hands during a typical eight-hour nursing shift, healthcare water consumption can be cut dramatically with touchless faucets.
There even are advanced hand-washing faucets designed to indicate minimum scrub time with visible reminders to ensure thorough hand-washing procedures are followed, no matter how busy the healthcare provider is.
With the amount of water saved by using low-consumption, sensor-operated products, even if LEED certification is not a stated goal of a project, knowledge of green design strategies will quickly pay off. (For more information, see next page.)
Improving Hygiene
Nosocomial infection - which means infections acquired in a hospital - is the fourth leading cause of mortality for Americans. According to the CDC, nearly 2 million patients in the United States are affected by nosocomial infections, and about 90,000 of these patients die as a result of their infection each year. The yearly infection mortality is more than car accidents, fires and drowning combined.These are frightening statistics and proof that building professionals should not be penny wise and pound foolish in selecting hand-washing equipment for hospitals. Although it may be thought that a faucet is just a means to access water, a review6 of public restrooms identified how much more hygienic sensor-operated fixtures are compared to manual units.
Isolating data for three types of facilities - hospitals, fast-food restaurants and high-traffic locations, like airports and schools - University of Arizona researchers took samples during a study to determine the dirtiest areas in a restroom.
The results showed that total coliforms (aerobic bacteria found in the colon or feces, often used as indicators of fecal contamination of water supplies) were present on 17.3 percent of the 248 surface samples taken from hospitals, which produced the lowest level of positive samples followed by fast-food restaurants (21.9 percent) and then high-traffic locations (23.8 percent).
In this study, researchers also learned the highest percentage of positive samples was in the area where people clean themselves. Sink drain surfaces resulted in positive samples of coliforms 80 percent of the time, followed by the rim of the sink (20 percent) and then the area under the soap dispenser (10 percent).
This is evidence that the installation of touchless plumbing fixtures will decrease the occurrence of nosocomial infections by significantly reducing the chain of contaminated elements a person touches in a hospital.
The chain of nosocomial infection, according to the CDC, begins when pathogenic organisms transfer to an individual by physical contact. In other words, a person is admitted to the hospital and later develops an infection possibly resulting from cross-contamination from a contaminated surface, which can include patient-to-surface contamination and hand-to-hand contact by visitors, medical personnel or any number of people involved in the care of a patient.
Approximately one-third of hospital-acquired infections are preventable, with the most effective method to reduce nosocomial infections being hand-washing. In fact, transfer of a pathogen to a patient via the hands of healthcare workers is thought to be the most likely mechanism of exposure to patients.
What is even more frightening is how easily a person can “pick up” and then transfer bacteria that can develop into a nosocomial infection.
It's a proven fact that a person who touches a contaminated surface can pass on the germs and bacteria just as easily. Clinical testing shows that cross-contamination can occur even up to 24 hours after original contamination7. Researchers at Rutgers, University found that the rate of cross contamination from a faucet to clean hands is as high as 72.4 percent8.
Additional research on cross-contamination concludes that the bacterial transfer rates of hand-to-hard surface are similar to the transfer rate of fingertips-to-the-lips,9 which is the final link in the chain - a portal of entry into a new host. Organisms will continue to transfer via touch until they are shed from the skin of the host or have been killed by antimicrobial agents.
Results like these exemplify the need to incorporate touchless plumbing fixtures into healthcare facilities to reduce nosocomial infections. Although hospital staffs are well trained to wash their hands - and most do a good job at meeting hospital standards - touching contaminated faucets or sinks after using the restroom or in between patients can negate the benefits of washing just as if the procedure was skipped.
References
1 DRAFT 2006: Guidelines for Design and Construction of Hospital and Healthcare Facilities (11/1/04). http://www.aia.org/aah_gd_hospcons2 DRAFT 2006: Guidelines for Design and Construction of Hospital and Healthcare Facilities (11/1/04). http://www.aia.org/aah_gd_hospcons
3 DRAFT 2006: Guidelines for Design and Construction of Hospital and Healthcare Facilities (11/1/04). http://www.aia.org/aah_gd_hospcons
4 DRAFT 2006: Guidelines for Design and Construction of Hospital and Healthcare Facilities (11/1/04). http://www.aia.org/aah_gd_hospcons
5 (**Boulder Community Foothills Hospital, LEED Silver Rating, Boulder, Colo. and The Patrick H. Dollard Discovery Health Center, Harris, N.Y., LEED Certified)
6 “Enteric Bacterial Contamination of Public Restrooms”
7 “Comparative surface-to-hand and fingertip-to-mouth transfer efficiency of gram-positive bacteria, gram-negative bacteria and phage”
8 “Quantification of Cross Contamination Rate Distribution”
9 “Comparative surface-to-hand and fingertip-to-mouth transfer efficiency of gram-positive bacteria, gram-negative bacteria and phage”
Study Captures Water Consumption
To fully understand water consumption in restrooms - particularly by lavatory faucets - a study was conducted at a major university that measured faucet consumption in four women's restrooms and four men's restrooms on four floors for a total of 16 lavatories.A new method to capture the frequency of use and calculate the amount of water consumed per event was developed by Texas A&M University to identify unique sound signals generated by individual plumbing fixtures.
Called AIRS, the Acoustic Information Retrieval System is a one-of-a-kind system consisting of multiple acoustic sensors attached to the water supply risers for each restroom.
Using the collected data, the AIRS software identifies fixture actuations, recording the time and duration of a specific, individual fixture actuation into a proprietary database for analysis.
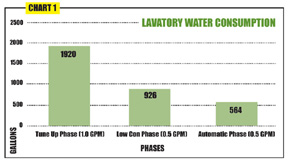
Using this method, water-use data was collected for approximately two weeks during the regular semester for three different phases of the study. These phases are identified as “Tune Up,” “Low Consumption” and “Automatic.” The fixture flow rate for fittings used during each phase of the study was measured in gallons and tabulated from flow duration in terms of seconds.
The study made certain assumptions:
- The use of average lavatory gallons-per-minute (gpm) across all fixtures will yield accurate gallons-per-day lavatory consumption.
- Unobserved fixtures will have little effect on the outcome.
Of course, this was not a problem with the automatic valve sets. Also, unlike a metered flushing fixture, the duration of a lavatory event could vary from one second to several minutes, pending how long the user chose to flow water. As a result, it was necessary to measure not only the frequency of use but also the duration. This meant measurement of the duration of each event required digital recording for data collection, hence AIRS.
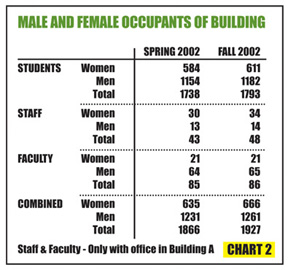
The total number of students, staff and faculty from semester to semester should give an indication of whether one could expect fixture event frequency to increase or decrease. Therefore, because there was about a 3 percent occupancy increase from spring to fall 2002, it was expected that there would be an increase in use over that period.
The nature of the experiment involved correlating different study periods, in which consumption is compared.
As you can see on the accompanying graphs, consumption during the Tune Up phase is the highest, with standard, manual activation faucets being used after calibration to original flow rates.
Predictably, during the Low Consumption phase that used low-consumption manual faucets, there was a significant decrease in consumption compared to the Tune Up phase.
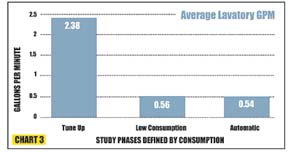
Documenting the amount of overall lavatory water use proved to be staggering, making the savings much more noteworthy, especially during the “Automatic” valve phase. The Automatic phase accounted for a 70 percent reduction relative to the original manual lavatory valve Tune Up phase; and there was a 39 percent reduction relative to the Low Consumption manual valve phase.
It is this last comparison that presents the most intriguing analysis: Even with calibrated flow rates being the same, low-consumption sensor-operated faucets - when compared to low-consumption manual faucets - reduce consumption significantly.